Clostridium difficile (C. difficile) infection (CDI) is a leading cause of antibiotic-associated diarrhea and a serious healthcare-associated infection (HAI) worldwide. Known for its high recurrence rates and resilience in the environment, CDI poses a major challenge for hospitals, long-term care facilities, and public health systems.
What is Clostridium difficile?
C. difficile is a Gram-positive, spore-forming, anaerobic bacterium. While it can live harmlessly in the intestines of some people, it becomes dangerous when the normal gut microbiota is disrupted often due to antibiotic use. Once overgrown, it produces Toxin A and Toxin B, which damage the intestinal lining, leading to inflammation and severe gastrointestinal symptoms.
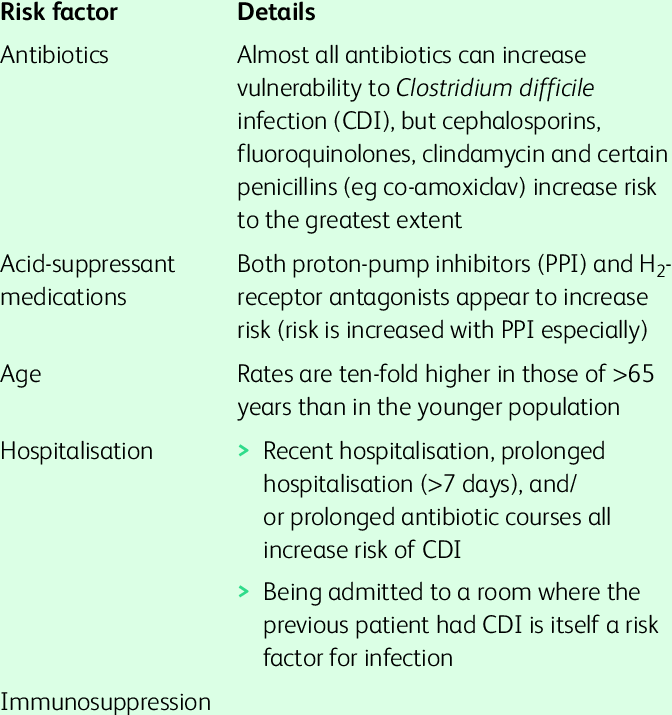
Causes and Risk Factors
The primary cause of CDI is exposure to C. difficile spores combined with changes in gut microbiota balance. Read more
Key risk factors include:
- Antibiotic use, especially clindamycin, fluoroquinolones, and cephalosporins
- Hospitalization or long-term care residence
- Advanced age (≥65 years)
- Weakened immune system due to illness or treatment
- Gastrointestinal surgery or procedures
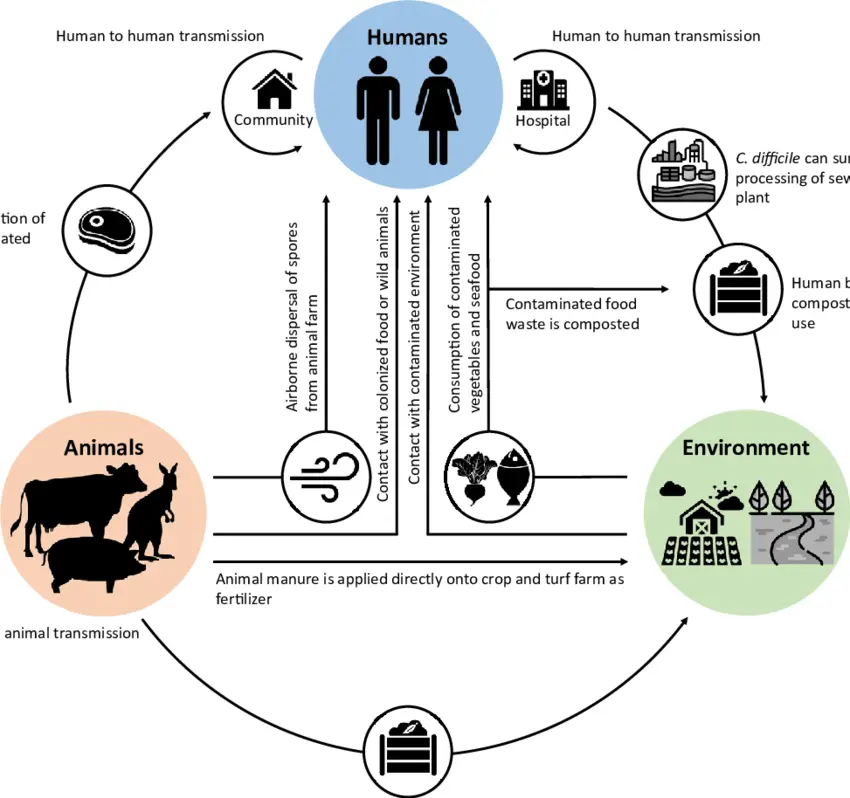
Transmission
C. difficile spreads through the fecal-oral route. Its spores can survive for months on surfaces such as bed rails, medical equipment, and clothing. Transmission typically occurs via contaminated hands, equipment, or surfaces in healthcare environments.
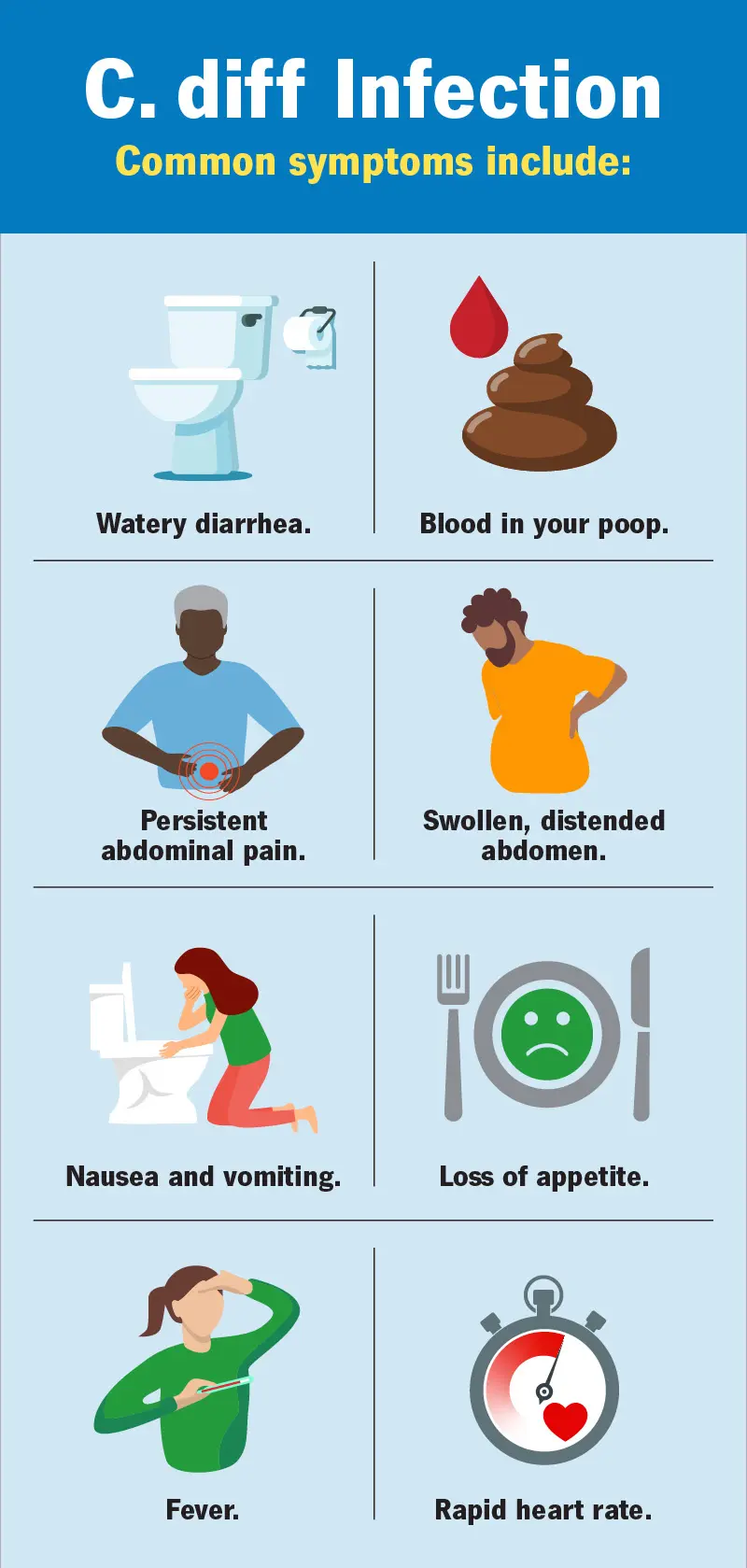
Symptoms of CDI
CDI can range from mild to life-threatening.
Common symptoms include:
- Watery diarrhea (three or more episodes per day)
- Abdominal cramping and tenderness
- Fever
- Nausea and loss of appetite
Severe cases may lead to:
- Pseudomembranous colitis
- Toxic megacolon
- Sepsis
Diagnosis
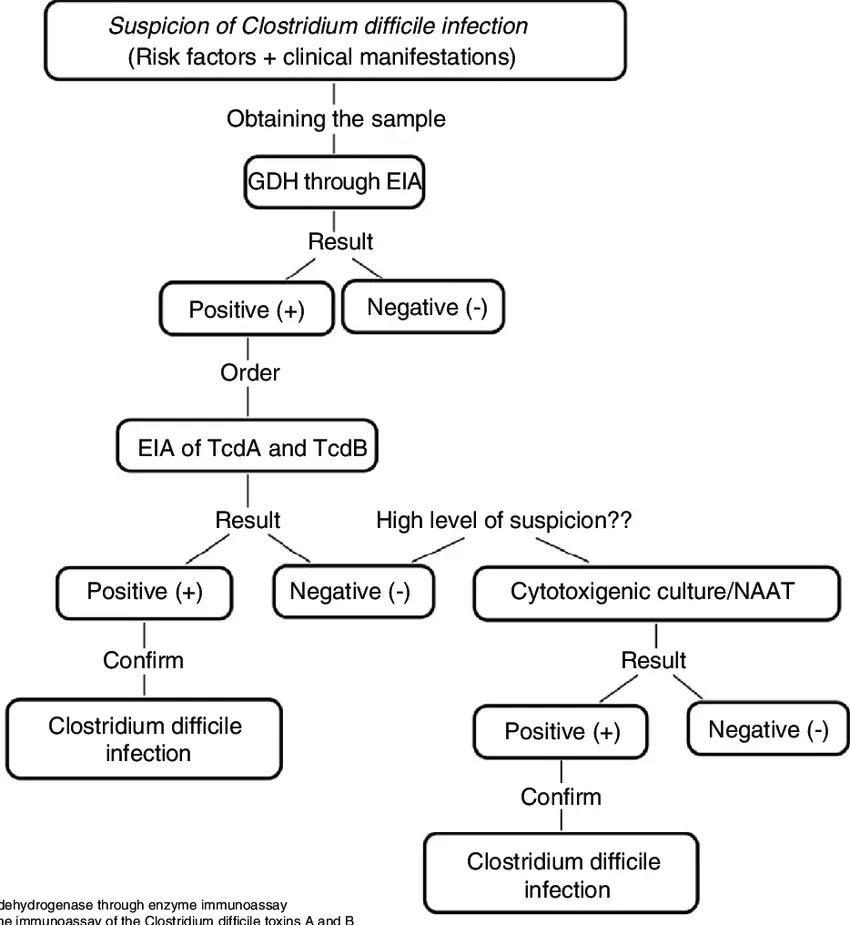
Accurate and rapid diagnosis is essential to prevent complications and limit spread.
Diagnostic methods include:
- GDH antigen testing (screening for C. difficile presence)
- Toxin enzyme immunoassays (EIA)
- Polymerase chain reaction (PCR) to detect toxin genes
- Colonoscopy in severe or unclear cases
Treatment Options
Treatment depends on severity:
- First-line antibiotics: Oral vancomycin or fidaxomicin
- Metronidazole: For mild cases if other options unavailable
- Fecal microbiota transplantation (FMT): Highly effective for recurrent CDI
- Probiotics: Under study as adjunct therapy
Prevention Strategies
Preventing CDI requires strict infection control and antibiotic stewardship:
- Rigorous handwashing with soap and water (alcohol gels do not kill spores)
- Environmental cleaning with sporicidal disinfectants
- Judicious antibiotic prescribing
- Isolation of infected patients in healthcare settings
Research and Outlook
Scientists are exploring:
- Vaccines against C. difficile toxins
- Monoclonal antibodies to prevent recurrence
- Microbiome restoration therapies
MetaPathogen provides researchers and healthcare professionals with access to up-to-date data, pathogen profiles, and learning resources to help combat CDI effectively.